
After the solar term in beginning of winter, the temperature plummeted. According to the annual clinical consultation, the risk of falls and fractures of the elderly will show an upward trend. This is related to environmental factors such as reduced activity in winter, thick clothes and slippery roads, and also related to physical factors such as aging and degeneration of various organs of the elderly. Today we will focus on the problem of osteoporosis. According to the epidemiological survey of osteoporosis in 2018, 6% of male patients with osteoporosis over 50 years old, 32.1% of female patients, and 51.6% of female patients over 65 years old in China. Our country not only has a high proportion of osteoporosis population, but also does not pay enough attention to osteoporosis. The bone mineral density of people over 50 years old is only 3.7%. In fact, both men and women have entered the early stage of bone loss since the age of 40, and we should prevent osteoporosis from this time.
1 minute self-examination of osteoporosis risk
By answering the 1-minute osteoporosis risk test of the International Osteoporosis Foundation, you can quickly know whether you have the risk of osteoporosis.
1. Parents have been diagnosed with osteoporosis or have been fractured after a light fall.
2. One of the parents has a hunchback.
3. The actual age is over 40 years old.
4. Is there a fracture due to a light fall in adulthood?
5. Do you often fall down (more than once last year) or worry about falling down because you are weak?
Has the height decreased by more than 3 cm after 6.40 years old?
7. Is it underweight (body mass index value is less than 19)
8. Have you ever taken steroid hormones such as cortisone and prednisone for more than 3 months (cortisone is often used to treat asthma, rheumatoid arthritis and some inflammatory diseases)?
9. Do you have rheumatoid arthritis?
10. Have you been diagnosed with gastrointestinal diseases or malnutrition such as hyperthyroidism or hyperparathyroidism, type 1 diabetes, Crohn’s disease or celiac disease?
11. Do you stop menstruating at or before the age of 45?
12. Have you ever stopped menstruating for more than 12 months except pregnancy, menopause or hysterectomy?
13. Did you have your ovaries removed before the age of 50 and didn’t take estrogen/progesterone supplements?
14. Do you often drink a lot (drink more than two units of ethanol every day, which is equivalent to 570ml of beer, 240ml of wine or 60ml of spirits)?
15. Currently used to smoking or used to smoke.
16. Exercise less than 30 minutes a day (including doing housework, walking and running, etc.)
17. Can’t you eat dairy products and don’t take calcium tablets?
18. Have you been engaged in outdoor activities for less than 10 minutes every day and have not taken vitamin D?
As long as the answer to one of the above questions is "yes", it is positive, suggesting the risk of osteoporosis, and suggesting bone mineral density testing or evaluating the risk of fracture.
Bone mineral density detection is suitable for the following groups
It is not necessary for everyone to do bone mineral density test. Compare the following self-test options to see if you need to have a bone mineral density test.
1. Women over 65 years old and men over 70 years old, regardless of other risk factors for osteoporosis.
2. Women under 65 and men under 70 have one or more risk factors for osteoporosis.
■ A slight collision or fall will cause a fracture.
■ Adults with low sex hormone levels caused by various reasons.
■ Those with diseases affecting bone metabolism or a history of using drugs affecting bone metabolism.
■ Patients receiving or planning long-term glucocorticoid treatment
■ Small and thin people
■ Long-term bedridden patients
■ People with chronic diarrhea
■ The answer to the 1-minute osteoporosis risk test is positive.
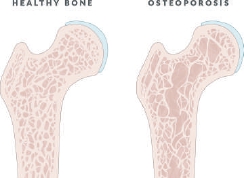
Normal osteoporosis
Remember "Five Origins and Three Stages" in Prevention and Control
The prevention and treatment of osteoporosis should follow five principles. First, increase bone mass and increase bone peak value; The second is to delay bone loss; Third, inhibit secondary hyperparathyroidism; The fourth is to prevent the first fracture; Fifth, reasonable dietary structure and nutritional composition ratio, quitting bad eating habits, increasing calcium intake, participating in moderate exercise and increasing sunshine.
Then, according to these five principles, the measures to prevent osteoporosis can be divided into three stages according to age: primary prevention, secondary prevention and tertiary prevention.
The primary prevention of osteoporosis is to start from childhood, to reach the highest bone mass (peak bone mass) in one’s life from childhood and adolescence to around 30-35 years old, with the goal of avoiding or alleviating the occurrence of osteoporosis as much as possible. There are mainly the following measures.
Reasonable dietary structure: milk is the most ideal calcium source, with 120mg of calcium per 100ml of fresh milk and a calcium absorption rate of 30%. The daily intake of calcium can be ensured by taking 500ml for adults, 750ml for children and 800ml for adolescents.
Choose foods with high calcium content: sesame sauce, shrimp skin, dried seaweed, kelp, milk, bean products and cheese are all foods with high calcium content.
Vitamin D intake: The daily intake of vitamin D is 400IU, and the vitamin D content in foods such as cod liver oil, canned sardines, egg yolk, shad and chicken liver is high. Sunlight irradiation is also one of the important ways to supplement vitamin D. Walking in soft sunshine for 40 minutes can ensure the vitamin D needed by the body. It is best to choose the irradiation time before 10 a.m. or after 3 p.m., so as to avoid too strong sunlight damaging the skin and eyesight.
Moderate exercise: participating in moderate exercise is helpful to increase bone mass and increase the peak bone mass.
Adhere to a healthy lifestyle: not addicted to alcohol and tobacco; Drink less coffee, strong tea and carbonated drinks; Less salt and less sugar.
When people reach middle age, they reach the secondary prevention stage of osteoporosis. The core of prevention at this stage is to delay the loss of bone mass in middle age and try to avoid the first osteoporotic fracture. Women aged 40-49 and men aged 40-64 enter the prophase of bone loss: the annual bone loss rate of women is 0.4%-0.6% and that of men is 0.3%-0.5%. Women enter the period of rapid bone loss 1-10 years after menopause, and the rate of bone loss is obviously accelerated, while men do not have the period of rapid bone loss. In addition to food supplement, physical exercise and a good lifestyle, the main preventive methods need to be supplemented with vitamin D and appropriate calcium. The recommended intake of vitamin D for adults is 400IU/d, and the maximum tolerable intake is 2000IU/d. When vitamin D is used for prevention and treatment of osteoporosis, the dosage is 800-1200IU/d..
The tertiary prevention of osteoporosis is the stage of mending after the sheep is dead, mainly aimed at the elderly, which is mainly reflected in inhibiting bone resorption, reducing bone turnover rate and preventing accidental injuries and fractures. Osteoporosis can be treated by supplementing calcium and vitamin D and taking anti-osteoporosis drugs under the guidance of professional doctors, so as to avoid osteoporotic fractures and re-fractures as much as possible.
Calcium supplementation alone cannot replace treatment.
The daily calcium intake standard recommended by China Nutrition Association is: 400mg; from birth to 6 months; 600mg; for 6-12 months; 800-1200mg; under 10 years old; 11-24 years old 1200-1500mg;; 1400mg; for pregnant or lactating women over 19 years old; Postmenopausal and postmenopausal women who did not take estrogen 1500mg;; Take estrogen 1000mg; for postmenopausal and postmenopausal women; Middle-aged male 1000mg;; 1000-1500mg for the elderly.
However, calcium supplementation alone cannot replace the treatment of osteoporosis. Osteoporosis patients can’t overcome the obstacle of calcium utilization by bones only by taking calcium orally, so they should be treated regularly under the guidance of doctors.
About 30% of elderly people over 60 years old and postmenopausal women have gastric acid deficiency. If they have flatulence and constipation after taking calcium carbonate, they should change to calcium citrate. The absorption of calcium citrate is independent of gastric acid and can prevent kidney calculi, which is especially suitable for those with gastric acid deficiency.
However, whether calcium supplementation is needed or not should be decided by consulting a specialist in a regular hospital and doing a bone mineral density examination. There is a threshold for calcium absorption. Excessive supplementation is not only a waste, but also can lead to kidney calculi’s disease, ectopic calcification and atherosclerosis. Kidney calculi, patients with advanced bone metastasis, hypercalcemia and cardiac and renal insufficiency are forbidden to supplement calcium.
(Author: Deputy Chief Physician, Center for Orthopedics, Osteoporosis and Bone Metabolic Diseases, Peking University Third Hospital)